August 21, 2018
New type 1 diabetes therapy shows promise for long-term reversal in both humans, dogs
WEST LAFAYETTE, Ind. — What if instead of daily insulin injections or wearing pumps, just getting a shot every few months could reverse Type 1 diabetes for you – or your dog?
It might take ushering in healthy pancreatic cells like a Trojan horse.
The Trojan horse, in this case, would be collagen, a protein that the body already makes for building muscles, bones, skin and blood vessels. A collagen formulation mixed with pancreatic cells, developed by Purdue University researchers in collaboration with the Indiana University School of Medicine, is the first minimally invasive therapy to successfully reverse Type 1 diabetes within 24 hours and maintain insulin independence for at least 90 days, a pre-clinical animal study shows.
For diabetic pets, the next step is a pilot clinical study in dogs with naturally occurring Type 1 diabetes, which will be conducted in collaboration with Purdue’s College of Veterinary Medicine.
"We plan to account for differences from mouse to human by helping dogs first. This way, the dogs can inform us on how well the treatment might work in humans," said Clarissa Hernandez Stephens, first author on the work and a graduate researcher in Purdue’s Weldon School of Biomedical Engineering. Findings appear in early view for a forthcoming issue of the American Journal of Physiology – Endocrinology and Metabolism.
 A new therapy is in a clinical stage of testing to reverse Type 1 diabetes in dogs, such as for 7-year-old Lexi, pictured next to her owner, Jan Goetz. (Purdue University image/Erin Easterling)
Download image
A new therapy is in a clinical stage of testing to reverse Type 1 diabetes in dogs, such as for 7-year-old Lexi, pictured next to her owner, Jan Goetz. (Purdue University image/Erin Easterling)
Download image
"With giving my dog shots twice a day, I have to constantly be thinking about where I am and when I need to be home. It greatly affects my work and my personal life," said Jan Goetz, owner of a diabetic dog named Lexi. "Not having to give these shots would mean freedom."
Type 1 diabetes affects about one in every 100 companion animals in the U.S., including dogs and cats, and approximately 1.25 million American children and adults.
David Taylor, an Indiana resident, has struggled with Type 1 diabetes for almost 50 years.
"A Type 1 diabetes diagnosis was my 18th birthday present, and since that first insulin injection, managing diabetes has been my 'other' full time job," Taylor said. "Treatment methods have improved enormously over 50 years, but they still permit no time off for the patient. Receiving an injection every few months would restore the near-normal life to me that I haven't had as an adult – and I could retire from that full-time diabetes management job."
Because diabetes in dogs happens similarly in humans, treatment has so far been largely the same: Both need their glucose to be monitored throughout the day and insulin to be administered after meals.
This also means that dogs and humans could potentially benefit from the same cure: A new set of pancreatic cells to replace the clusters of cells, called islets, that aren't releasing insulin to monitor blood glucose levels. A YouTube video is available at https://youtu.be/vndD_U2gb5Q.
Still, 20 years of research and clinical trials hasn't produced an effective islet transplantation therapy because multiple donors are needed, the current method of delivering islets through the portal vein of the liver is too invasive and the human immune system tends to destroy a large percentage of transplanted islets.
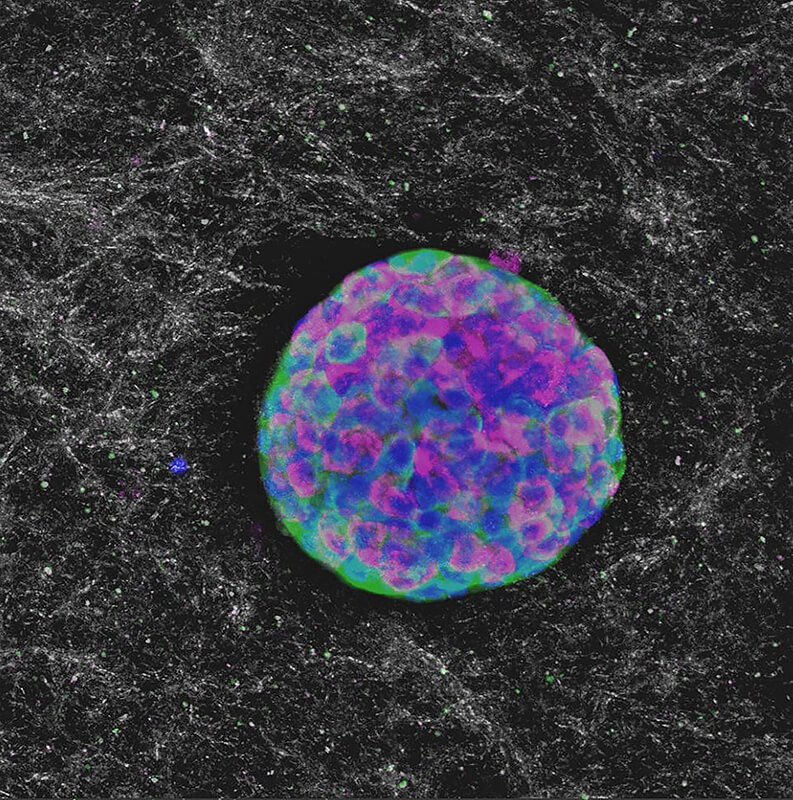 Purdue researchers in collaboration with the IU School of Medicine successfully injected a collagen solution mixed with pancreatic cells into diabetes-induced mice, achieving normal glucose levels for at least 90 days. (Purdue University image/Clarissa Hernandez Stephens)
Download image
Purdue researchers in collaboration with the IU School of Medicine successfully injected a collagen solution mixed with pancreatic cells into diabetes-induced mice, achieving normal glucose levels for at least 90 days. (Purdue University image/Clarissa Hernandez Stephens)
Download image
Purdue researchers simply changed how the islets were packaged – first, within a solution containing collagen, and second, as an injection through the skin instead of all the way at the liver, saving patients from a nasty procedure.
"Traditionally, we transplant islets in the liver of the animal and never do it under the skin, in large part because the skin doesn't have the blood flow that the liver has for transporting insulin released by islets. And there are a lot of immune cells in the skin, so chances of rejection are high," said Raghu Mirmira, professor of pediatrics and medicine and director of the Diabetes Research Center at the Indiana University School of Medicine.
The team removed the need for transplanting in the liver by thoroughly mixing mouse islets, provided by Mirmira's lab, with the collagen solution. Upon injection just under the skin, the solution solidifies, the body recognizes the collagen and supplies it with blood flow to exchange insulin and glucose.
"It's minimally invasive; you don't have to go to the operating room and have this infusion into the portal vein. It's as easy as it comes, just like getting a shot," said Sherry Voytik Harbin, Purdue professor of biomedical engineering and basic medical sciences.
The researchers tested the effects of the solution between mouse twins and non-twins to check for discrepancies. Initial studies showed if the mouse donor were a twin to the recipient, the diabetic mouse could go at least 90 days without needing another shot. If not twins, the mouse would have normal blood sugar levels for at least 40 days. Nearly all transplanted islets survived either scenario, removing the need for multiple donors to compensate for those killed off by the immune system.
As they transition to testing the formulation in naturally diabetic dogs, the researchers will explore the feasibility of transplanting pig islets or stem cells programmed to produce insulin, in hopes that either method will further increase donor availability.
The islet transplantation therapy might also have implications for better treating severe pancreatitis.
Purdue and the IU School of Medicine collaborated on this work through the National Institute of Health T32 Indiana Bioengineering Interdisciplinary Training for Diabetes Research Program, which awarded a fellowship to Stephens to develop innovative technology for the treatment of diabetes.
The collagen formulation is a patented technology. This research was also supported by the National Science Foundation Graduate Research Fellowship (DGE-1333468); the Indiana University School of Medicine Center for Diabetes and Metabolic Diseases Pilot and Feasibility Program (P30DK097512); and generous donations from the McKinley Family Foundation. The study utilized core services provided by NIH grant P30 DK097512 to the Indiana University School of Medicine.
Writer: Kayla Wiles, 765-494-2432, wiles5@purdue.edu
Sources: Sherry Voytik Harbin, 765-496-6128, harbins@purdue.edu
Clarissa Hernandez Stephens, herna171@purdue.edu
Raghu Mirmira, rmirmira@iu.edu
Note to Journalists: For a full-text copy of the paper, or to speak with the researchers or the Type 1 diabetes patient quoted in the release, please contact Kayla Wiles, Purdue News Service, at wiles5@purdue.edu. A YouTube video is available at https://youtu.be/vndD_U2gb5Q, and other multimedia can be found in a Google Drive folder at https://goo.gl/bTGnRA. The materials were prepared by Erin Easterling, digital producer for the Purdue College of Engineering, 765-496-3388, easterling@purdue.edu.
ABSTRACT
In-situ type I oligomeric collagen macroencapsulation promotes islet longevity and function in vitro and in vivo
Clarissa Hernandez Stephens1, Kara S. Orr2, Anthony J. Acton2, Sarah A. Tersey2, Raghavendra G. Mirmira2, Robert V. Considine2, and Sherry L. Voytik-Harbin1
1Purdue University, West Lafayette, IN, USA
2Indiana University School of Medicine, Indianapolis, IN, USA
https://doi.org/10.1152/ajpendo.00073.2018
Widespread use of pancreatic islet transplantation for treatment of type 1 diabetes (T1D) is currently limited by requirements for long-term immunosuppression, limited donor supply, and poor long-term engraftment and function. Upon isolation from their native microenvironment, islets undergo rapid apoptosis, which is further exacerbated by poor oxygen and nutrient supply following infusion into the portal vein. Identifying alternative strategies to restore critical microenvironmental cues, while maximizing islet health and function, are needed to advance this cellular therapy. We hypothesized that biophysical properties provided through type I oligomeric collagen macroencapsulation are important considerations when designing strategies to improve islet survival, phenotype, and function. Mouse islets were encapsulated at various Oligomer concentrations (0.5 to 3.0 mg/mL) or suspended in media and cultured for 14 days, after which viability, protein expression, and function were assessed. Oligomer-encapsulated islets showed a density-dependent improvement in in-vitro viability, cytoarchitecture, and insulin secretion, with 3 mg/mL yielding values comparable to freshly isolated islets. For transplantation into streptozotocin-induced diabetic mice, 500 islets were mixed in Oligomer and injected subcutaneously, where rapid in-situ macroencapsulation occurred, or injected into saline. Mice treated with Oligomer-encapsulated islets exhibited rapid (within 24 hours) diabetes reversal and maintenance of normoglycemia for 14 (immunocompromised), 90 (syngeneic), and 40 days (allogeneic). Histological analysis showed Oligomer-islet engraftment with maintenance of islet cytoarchitecture, revascularization, and no foreign body response. Oligomer-islet macroencapsulation may provide a useful strategy for prolonging the health and function of cultured islets and has potential as a subcutaneous injectable islet transplantation strategy for treatment of T1D.

