Neurophysiology and Neuroplasticity Studies
Swallowing is a complex biological function that is controlled by six pairs of cranial nerves and many areas/centers in the brainstem and brain. Disruptions in any of the complex swallowing neural pathways may lead to difficulty swallowing (also known as dysphagia).
The series of swallowing neurophysiology and neuroplasticity studies conducted by our team aim to help us better understand the underlying central and peripheral neural mechanisms that control this vital human function, in an effort to inform clinical decisions and develop neurophysiologically-driven treatments.
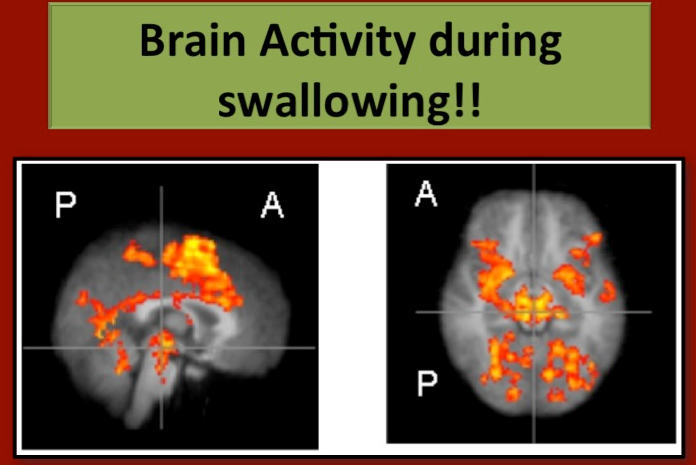
Brain activity during swallowing in healthy young adults
Our early swallowing neurophysiology work focused on providing insights on the underlying neural mechanisms of swallowing function in healthy adults (Malandraki et al. 2009; Malandraki et al. 2010; Malandraki et al. 2011; Paine et al. 2011). Based on this work our team was among the first to identify areas of the brain responsible for different aspects of the swallowing sequence, thus providing insights on functional specificity and further validation for the role of the brain (cortex and subcortex) in swallowing control.
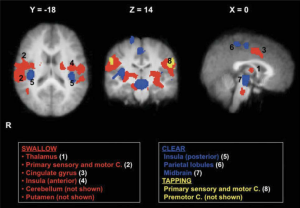
Areas of most significant activation during swallowing (shown in red), during throat clearing (shown in blue), and during tongue tapping (shown in yellow). (Malandraki et al. 2009)
Developmental Neuroplasticity of Swallowing and Speech – CP study
One of our largest studies (funded by NIH and AACPDM) has been focused on examining the neuroplastic adaptations of swallowing and speech in school age children with unilateral and bilateral brain damage manifesting as cerebral palsy (CP).
In essence by investigating the behavioral, peripheral, and central neurophysiological profile of these children we have started gaining a better understanding of how the central and the peripheral nervous systems adapt for several functions, such as feeding, swallowing, and speech after early brain lesions. This understanding is imperative in our efforts to develop new and better treatments for feeding, swallowing, and speech for these children who currently remain largely under-treated in these domains. This study is partially supported by the NIH (NIDCD) and the American Academy of Cerebral Palsy and Pedal-with-Pete Foundation.
These studies are now closed to recruitment and data analyses is in progress. Several manuscripts are under review or in preparation and will become available as soon as they are published. If you have any questions about these studies please contact us at swallowinglab@purdue.edu.
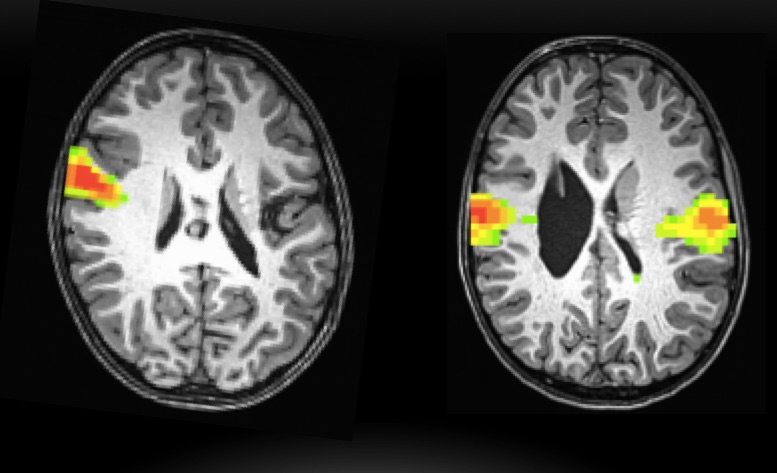
Sensorimotor network at rest of two children with unilateral CP. Our preliminary studies show that children with bilateral sensorimotor resting networks (as shown on the right image) may have more severe clinical signs of dysphagia than children with contralesional sensorimotor resting networks (shown on the left image) (Malandraki et al. 2017, ESSD).
Determining the Relationship between Swallowing and Speech Across the Lifespan
The aerodigestive system is shared for several critical functions, including the functions of swallowing and speech. A series of related research studies of our lab in this area involve the investigation of the neurodevelopment and cross-system interactions of swallowing and speech in typically developing children, as well as in young and older adults. In pediatrics these studies are in collaboration with Dr. Lisa Goffman (UT-Dallas, Texas) and co-led by PhD candidate Rachel Arkenberg and Dr. Malandraki. In adults these studies are in collaboration with Dr. Huber and the Purdue Motor Speech Lab. Our goal with these studies is to better understand the control of these functions, their potential cross-system relationships, and the potential inter-play between them in daily situations (eg., during eating a meal), in order to determine new and potentially cross-system interventions for swallowing and speech disorders.
The pediatric study is closed to recruitment at this stage. Analyses and manuscript preparation are under way. The adult study has been halted and will resume in fall of 2022. If interested to learn more about either of these exciting studies, please contact us at swallowinglab@purdue.edu or (765) 496-0207.

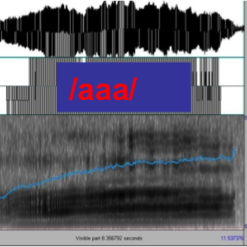
Determining the Relationship between Swallowing and Voice
Research has shown that the functions of swallowing and voice production (particularly pitch elevation) share anatomical and neurophysiological substrates. In our earlier preliminary research in this area we showed that reduced pitch elevation can be indicative of reduced airway protection in some dysphagia patients (Malandraki et al. 2011). More recently our team revealed that reduced ability to elevate vocal pitch was actually predictive of silent aspiration of small liquid volumes with high sensitivity and moderate specificity in a sample of stroke patients (Rajappa et al. 2017).
Although these findings are promising and have started shedding light into how these cross-system interactions can be utilized, the exact neurophysiological and biomechanical correlates between the two functions are still not very well understood.
Our recently completed study (Venkatraman at el., 2020), funded by the Dept of Speech, Language, & Hearing Sciences, identified that these two functions have similar anterior but not superior hyoid displacement, indicating that swallowing and pitch elevation have some shared biomechanics underlying them, which may explain the clinical findings in our prior work.
We are now in the process of using Computational Analysis of Swallowing Mechanics (CASM) in collaboration with Dr. Bill Pearson to further explore this dataset.
The next step in this important research should explore whether pitch elevation can provide any therapeutic benefit to swallowing disorders.
To learn more about this study contact us at swallowinglab@purdue.edu.

Students/trainees involved in these studies (now or in the past)
- Rachel Arkenberg
- Samantha Mitchell
- Anny Alvar
- Anumitha Venkatraman
- Kara Simon
- Kausar Abbas
- Tom Lu
- Lucia Figueiredo-Mourao
- Naomi Dreyer
- Pratik Kashyap
- Cagla Kantarcigil
Funding provided by:
- National Institute on Deafness and Other Communication Disorders (NIDCD, NIH) [Early Career R21, PI: Malandraki]
- American Academy of Cerebral Palsy and Developmental Medicine and Pedal-with-Pete Foundation [PI: Malandraki]
- Department of Speech, Language, & Hearing Sciences [student grant]
- Seed MRI fund, College of Health and Human Sciences, Purdue University [PI: Malandraki]
- Indiana Lions McKinney Outreach Program [student grant]
- National Institutes of Health / Eunice Kennedy Shriver National Institute of Child Health and Human Development [R01, PI: Friel]










