Purdue psychological sciences researcher ignites understanding of vagus nerve’s role in gastroparesis through NIH’s SPARC initiative

Purdue Psychological Sciences Professor Terry Powley sits in front a powerful microscope he has used to study the vagus nerve for years.Tim Brouk
Written by: Tim Brouk, tbrouk@purdue.edu
A six-year, $13.5 million study of the vagus nerve’s connection from the brain to the stomach has ignited interest from Indiana gastroenterologists and their hundreds of patients suffering from gastroparesis, a health condition where the stomach does not empty appropriately. When the stomach does not empty properly it can lead to serious health problems such as dehydration, malnutrition and bezoars, or hardened masses of food that can block the digestive tract. The vagus nerve involuntarily stimulates muscles of the stomach to contract for normal stomach emptying, and more information about how it functions will be helpful in identifying treatments for health conditions like gastroparesis.
The Purdue University-driven “Mapping Stomach Autonomic Circuitry and Function for Neuromodulation of Gastric Disorders” project has contributed new findings and collaborations as part of the National Institutes of Health’s SPARC (Stimulating Peripheral Activity to Relieve Conditions) initiative. This translational research study examines the connection between nerves like the vagus and major organs like the stomach. Understanding nerves’ interactions with organs can better control and regulate function in those suffering from diabetes, hypertension and gastrointestinal disorders like gastroparesis.
Terry Powley, a distinguished professor in the Department of Psychological Sciences, has studied the “wandering” and complicated vagus nerve for decades. He is among a packed roster of researchers, anatomists and physicians from Purdue and far beyond West Lafayette who have experimented with electrode and stimulator surgical implants on the stomachs of those suffering from gastroparesis.
The international study includes faculty and physicians from the Purdue College of Engineering and Indiana University-Purdue University Indianapolis (IUPUI) as well as researchers from the University of Melbourne and Flinders University in Australia, the University of Auckland in New Zealand, Indiana University School of Medicine, and Mount Sinai Hospital in New York.
Powley collaborated with IU School of Medicine gastrointestinal doctors in gathering data on gastroparesis patients and a healthy population. He and his collaborators studied MRI and fMRI (functional magnetic resonance imaging) scans of the participants’ esophagi and stomachs in the form of 4D stills and real-time video.
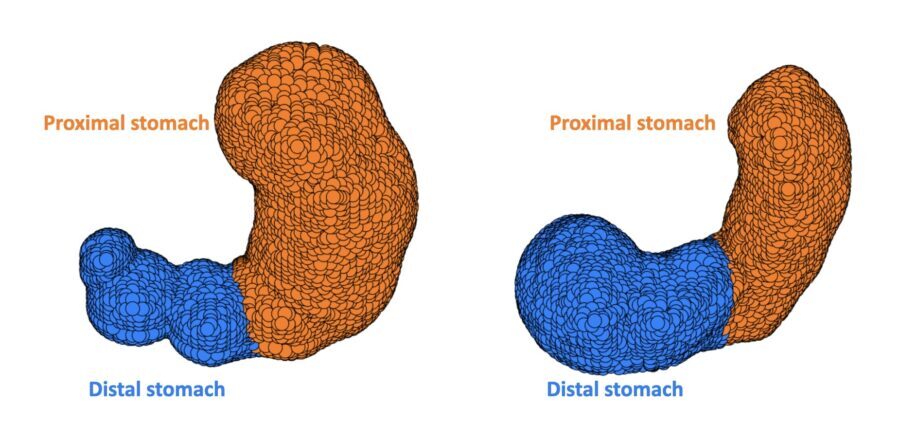
Powley and this team have developed 4D renderings of the stomachs of a healthy participant, left, and a patient suffering from gastroparesis, right.Provided by Terry Powley
Epilepsy treatment inspiration
Electrode and stimulator development for gastroparesis was encouraged by electrode treatment on the vagus nerve for patients with drug-resistant epilepsy. These patients experienced positive results with electrodes implanted in their necks, a major intersection for the vagus’ widespread circuitry up and down the body.
Just how much stimulation to the vagus nerve is needed to treat gastroparesis depends on the patient. One stimulation level or electrode placement on the stomach that might show positive results in one patient probably won’t in the next.
“The stomach is a complicated organ and not all parts are same or equal,” Powley said. “If you put the electrode in one place you might get one effect, a different place a different effect.”
‘We have moved the needle’
Like most neuroscientists, Powley started with brain research. After years of delving into the vast neural network of the human brain, he found working with the vagus nerve to be more interesting. He saw a better chance in making an impact in improving human health.
Powley found the vagus to be “anything but a cable,” meaning impulses fly up and down and all around the body from the nerve, thanks to its heterogenous axons or nerve fibers. Understanding the vagus is crucial in stimulation therapies because other nerves are like direct cables.
“You have to tune your stimulation differently for the stomach as opposed to the heart, for example,” Powley said. “Before SPARC, I thought the stimulation that was being done to the nerve was so primitive. I call it first-generational. The bulk of the work hasn’t kept up with what we know about the nerve.”
Since SPARC, Powley and his colleagues have brought more understanding to the nerve and how it can be best stimulated. The research has covered the where, why and how.
“We’ve been able to find the neural code to better tune the stimulation,” Powley reported. “If you happen to have a stomach that is misbehaving, we can very particularly prescribe what’s wrong, where to look, what to do and what (stimulation) tune to use.
“We have moved the needle in terms of the therapeutic applications of the vagus.”
Beyond an empty stomach
While Powley’s SPARC role focuses on the stomach, the research can have applications to diseases and disorders of the liver, lungs, spleen and kidneys.
Treatment is the ultimate SPARC goal but the last five years of this project have garnered more understanding of the vagus nerve, including its structure via electron microscopy.
“That’s never been done before,” Powley said. “Looking at the nerve in such detail could aid organ donor surgeons. When they get the organ for transplant, the tissue will have pieces of the vagus with it. It’s very much all wound together with clinical applications and so forth.”
Powley’s focus on gastroparesis has the attention of IU Health. The Indiana healthcare system’s gastrointestinal physicians report gastroparesis is the most common ailment they see.
“The stomach’s not behaving itself, and when it doesn’t, that creates a lot of havoc, and you’re not a comfortable person,” Powley said. “There are numerous ways to try to fix it, but there’s a lot not yet known about it. Through this project, we’ve gone through a thorough characterization of the physiology and anatomy and how it functions. With imaging, we’re able to say, ‘Here’s what to look for and here’s where to put an electrode in and stimulate like this.’ We can now be more concrete, specific and data-based.”
The SPARC experience has brought a new chapter to Powley’s vagus nerve research.
“I’ve been working on the basic science of the vagus for years and years, and now it’s an opportunity to see the implications of it,” he said. “It’s terrific to collaborate with a lot of people who really bring these other skills to it. I think it’s a productive kind of synergy you get when you put the pieces together and see what’s going on. For me, it’s a natural progression but a nice progression.”
The initial $10 million SPARC grant was awarded in 2016. A $3.5 million extension was granted in 2021 and runs through July 31, 2022. Three more years could be in the works.