Health through engineering and analytics.
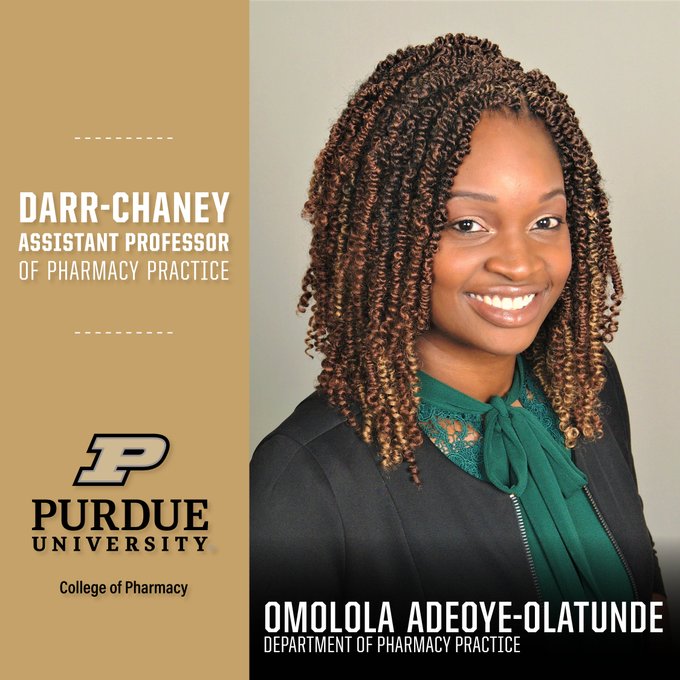
Congratulations to Dr. Omolola Adeoye-Olatunde, who has been named the Darr-Chaney Assistant Professor of Purdue College of Pharmacy.
Dr. Omolola (Lola) Adeoye-Olatunde has been named the Darr-Chaney Assistant Professor of Purdue College of Pharmacy.
Health
Systems
Health
Data Science
Population Health
and Health Equity
Health Communication
and Education
Research
Education
Impact & Partnerships
Subcenters
News and Announcements
Dr. Pavlos Vlachos is awarded rare honor from the American Heart Association

RCHE Faculty Leadership member Petros Drineas named Fellow by the Society for Industrial and Applied Mathematics
